You will be able to:
- Understand the indications for visualising the abdominal aorta with ultrasound
- Identify normal abdominal vascular anatomy.
- Follow the course of the Abdominal aorta from diaphragm to bifurcation sonographically.
- Identify aneurysmal and early aneurysmal changes.
- Recognise limitations and pitfalls of aorta ultrasound.
Introduction
- AAA rupture is 10th leading cause of death in males >50ys
- Mortality rate following rupture approaches 90%
- Physical exam often unreliable
- Abdo palpation has 68% sensitivity in detecting AAA
- Classic triad uncommon
- Fast, easy and cheap
- ED physicians can detect AAA rapidly with up to 100% accuracy after minimal training
Indications
The presence of:
- syncope
- shock
- hypotension
- abdominal pain
- abdominal mass
- flank pain
- back pain......especially in the older population.
INTRODUCTORY SONOSITE ABDOMINAL AORTA EXAM
AAA EXAM (5MIN SONO)
Anatomy
•Aorta passes through diaphragm at T12 (xiphoid process)
•Runs L of mid line for approx. 13cm
•Bifurcates at approx L4 (umbilicus)
Major branches
1.Coeliac Trunk
- Just below diaphragm
- Y-shaped fork (Hepatic A/Splenic A)
- Seagull sign
2.Superior Mesenteric Artery (SMA)
- 1cm below coeliac trunk
- Runs anterior and parallel to aorta in caudal direction
- Good point for a “suprarenal measurement”
3.Renal Arteries
- Distal to SMA
- Usually not seen in sagittal views
- <3cm from diaphragm
- 90% of aneurysms originate distal to this point
Technique for scanning
- Curvilinear probe
- Abdominal preset
- Gel+++
- Explain procedure including “limited scan” concept
- Position patient
Orientation
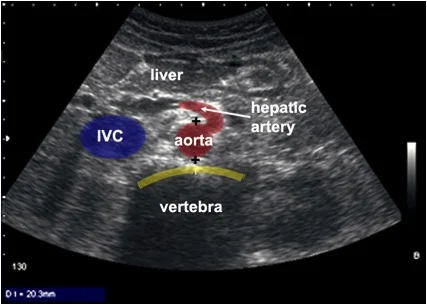
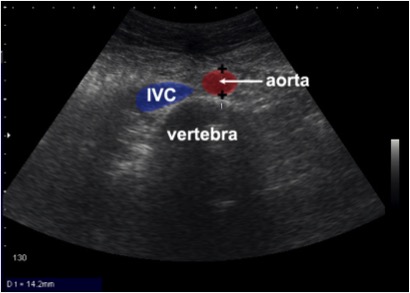
•Start in the transverse plane (pointer to “9 o’clock”), high in the epigastrium, using the liver as a sonic “window”.
•Identify the vertebral body
•Identify the aorta
•IVC (patient’s right) “above” the vertebral body on the ultrasound image.
•Obtain transverse images of the aorta from the coeliac to the bifurcation.
•Optimise image
3 Transverse views of the Aorta
Proximal (Coeliac Trunk level)
Mid (SMA level)
Distal Aorta & Bifurcation
PLUS
Longitudinal view (if possible from the coeliac to the bifurcation)
One view should show the maximal aortic diameter.
Obtain views of Common Iliacs where possible
'SEA GULL SIGN'
•If the gas-filled transverse colon obscures the aorta move the probe until you find a sonographic window between loops of bowel:
•Rock the probe up and down without moving it across the patient’s skin to maximize the information attained through the “window”.
•Frequently identifiable “sonic windows” in the upper abdomen include:
–high in the epigastrium.
Ask the patient to “take a deep breath and hold” to lower the liver margin.
If an AAA is identified...
- How big?
- Is there free fluid?
Aortic Pathology
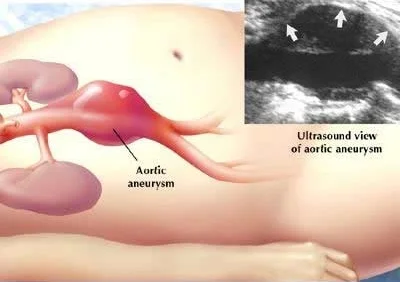
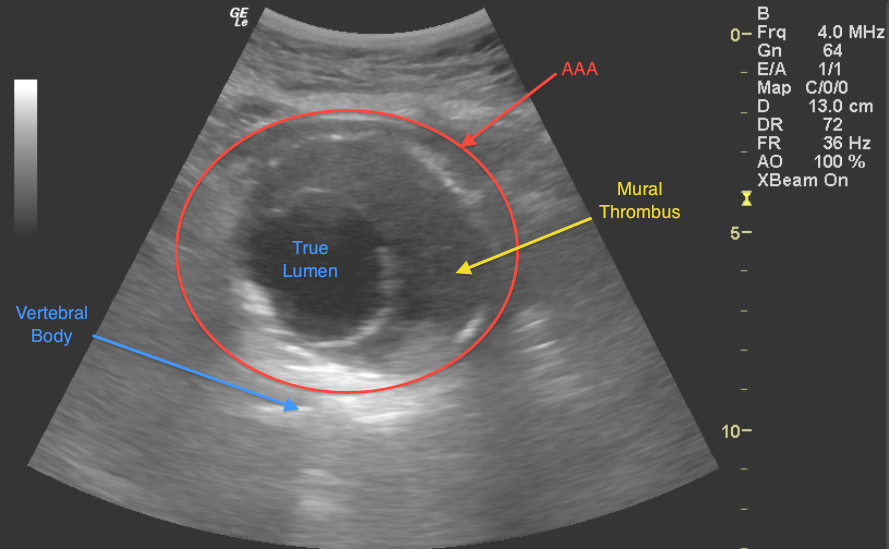
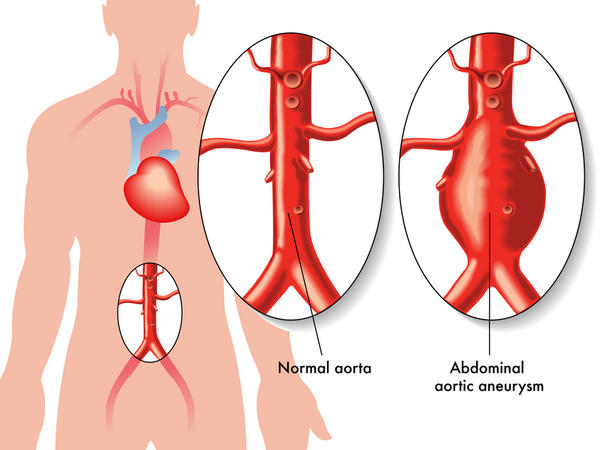
•An AAA is described as being a focal dilatation of the abdominal aorta of 150% of normal.
•Conventionally, an AAA is diagnosed when the diameter exceeds 3.0 cm.
•Risk of rupture for an AAA of 3.0 cm is less than 4% over 5 years; this risk, however, substantially increases for AAA’s with larger diameters.
•A true aneurysm by definition involves dilation of all three layers of the aorta: Intima, media, and adventitia.
Top Tips
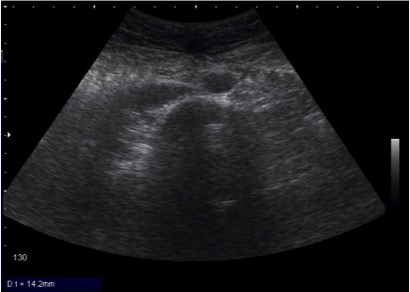
- Obtain measurements of the aorta from outer wall to outer wall. Since aneurysms will often contain a thrombus, one may accidentally mistake the inner rim of the thrombus for the aortic wall. Doing this will lead a falsely decreased measurement of the true aortic diameter.
- Avoid oblique or angled cuts if possible, especially with a tortuous aorta, which will exaggerate the true aortic diameter.
- A small aneurysm does not preclude rupture. Any symptoms consistent with rupture in a patient with an aortic diameter greater than 3.0 cm should have this diagnosis (or alternative vascular catastrophes) ruled out.
- Scanning should be systematically performed in real-time from the diaphragmatic hiatus to the bifurcation in order to avoid missing small, localized saccular aneurysms.
- Although axial resolution is usually greater than lateral resolution, transverse views are needed because many AAAs have larger transverse than AP diameter.
- The majority of aneurysms are fusiform, affecting the entire circumference of the vessel. Saccular aneurysms are uncommon and affect only part of the aortic circumference.
Problems/Pitfalls
- The Fat patient? 3.5 probe and depth _ Does your machine go deep enough, Penetration settings
- Is it aorta or IVC or superior mesenteric?
- Gas in the way! Not starved and air swallowing – Controlled pressure and jiggle and wait.
- Just can’t see it? Get the patient to bend their knees or try Left lateral view
- Accuracy of measurement – measure in 2 views